Tooth whitening lightens natural teeth by using peroxide-based gels that break down stain molecules inside enamel and dentin. Professional and dentist-supervised options are usually more predictable than DIY trends. The most common side effect is temporary sensitivity, and fillings or crowns won’t whiten so a dental check helps you choose a safe method and a natural-looking shade.

Tooth colour changes for two main reasons: surface stains (coffee, tea, smoking) and deeper colour changes within the tooth. Whitening targets both, but it works best on natural tooth structure.
Most evidence-based whitening relies on hydrogen peroxide or carbamide peroxide. These ingredients can penetrate tooth tissues and oxidise stain compounds, which is why they can brighten beyond what a “whitening toothpaste” can do.
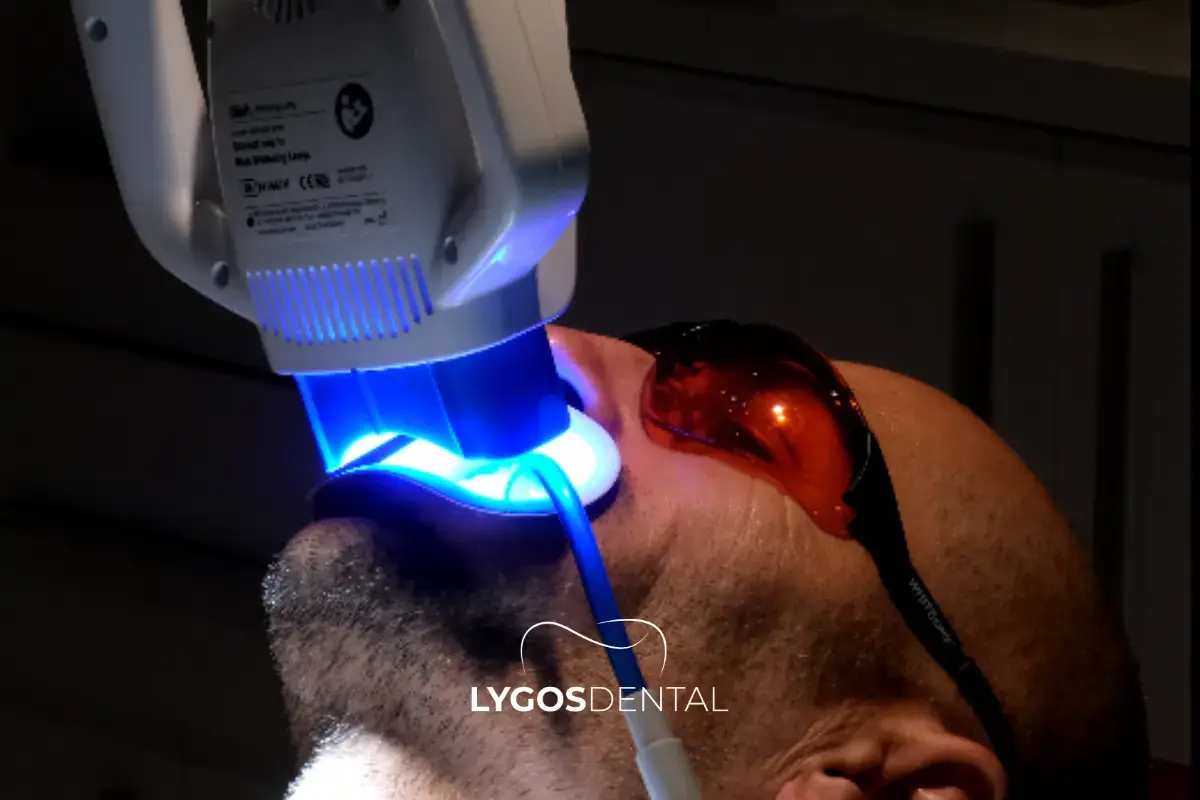
In-office whitening typically uses higher-concentration gels applied with gum protection and clinical supervision. The upside is speed and professional control over soft-tissue safety. The trade-off is that sensitivity can be more noticeable, especially in the first 24–48 hours.
If you’re prone to sensitivity, dentists often adjust concentration, exposure time, or choose a staged plan rather than pushing for a dramatic jump in a single visit.
Custom trays with dentist-provided gel are a “quietly powerful” option: slower than in-office, but often very even and easier to fine-tune. Many patients like this route because it’s more controllable day-to-day.
For people who want a natural improvement (instead of an ultra-bright change), trays are often the most flexible.
Whitening strips can work for mild to moderate staining, especially if used consistently. Results vary more than professional options because one-size-fits-all trays and generic instructions don’t account for your tooth shape, gum line, or existing sensitivity.
One practical rule: if a product burns your gums, feels sharp on exposed root areas, or spikes sensitivity early, stop and get advice.
Most “whitening toothpastes” mainly remove surface stains through gentle abrasives and polishing agents. They can make teeth look cleaner and brighter, but they don’t usually change the underlying shade the way peroxide gels can.
They’re best viewed as maintenance, not a substitute for true bleaching.
Light-activated whitening is heavily marketed. The research picture is mixed: some studies show limited added benefit compared with peroxide alone, and results depend on the gel formula and protocol.
If you’re choosing professional whitening, the clinician’s technique and diagnosis usually matter more than whether a lamp is used.
The #1 complaint is short-term sensitivity (cold air, cold drinks). It typically settles within days. Using a desensitising toothpaste, spacing sessions, and choosing a lower-strength plan can help.
If you already have sensitivity, whitening can still be possible but it should be planned around the cause (enamel wear, gum recession, cracks, or decay).
Gel that leaks onto the gums can irritate soft tissue. Custom trays and professional barriers reduce this risk. If your gums turn white briefly during whitening, that’s often a sign of chemical irritation from gel contact another reason fit matters.
Peroxide whitening, when used as directed, is considered safe and effective.
What tends to cause trouble is misuse: over-wearing trays, using high-strength gels too often, or combining multiple products aggressively.
Be cautious with abrasive “hacks.” Charcoal-based whitening products, for example, have been linked in studies to increased enamel roughness/abrasion and limited true whitening benefit.
A dental exam is especially important if you have:
Also, regulations vary by country, but in many places whitening products above certain peroxide levels are restricted to dental professionals, and cosmetic whitening for under-18s is generally not allowed.

The most believable smiles usually brighten by a few shades, not ten. A dentist can help you pick a target shade that matches your skin tone and eye whites, and avoids the greyish or overly opaque look some people get when they push too far.
Crowns, veneers, bonding, and tooth coloured fillings do not change colour with whitening.
If you have front-tooth restorations, the usual strategy is: whiten first, then replace or adjust restorations (if needed) to match the new shade.
Longevity depends on habits and maintenance. Coffee/tea, red wine, smoking, and poor brushing shorten results. Many people do quick “top-ups” (often with trays) rather than repeating full-strength whitening.

Before you spend money on kits or sessions, make sure you know:
A short dental appointment can prevent weeks of trial-and-error.
You can contact us here to learn more about Cosmetic Dentistry, Dental Crown, Dental Implant and General Dentistry to make an appointment and to get information about our services.
For most healthy adults, peroxide-based whitening is considered safe when used correctly. The most common side effect is temporary sensitivity.
In-office whitening can show results the same day. Take-home trays and strips typically improve shade over 1–2 weeks, depending on the product and starting colour.
No only natural tooth structure whitens. If restorations are visible when you smile, you may need a plan to match them after whitening.
Sensitivity happens when whitening temporarily increases fluid movement in the tooth. It usually fades within a few days. Desensitising toothpaste and gentler protocols often help.
They may remove some surface staining, but evidence suggests limited true whitening and potential enamel roughness/abrasion with charcoal products.
Special Note:
Our treatments are provided by healthcare facilities that possess a health tourism authorization certificate
Special Note: Our treatments are provided by healthcare facilities that possess a health tourism authorization certificate
Selenium Retro, Ataköy 7-8-9-10. Kısım, D-100 Güney Yanyolu No:18/A, 34158 Bakırköy/İstanbul
© 2025, LYGOS DENTAL. All Rights Reserved.